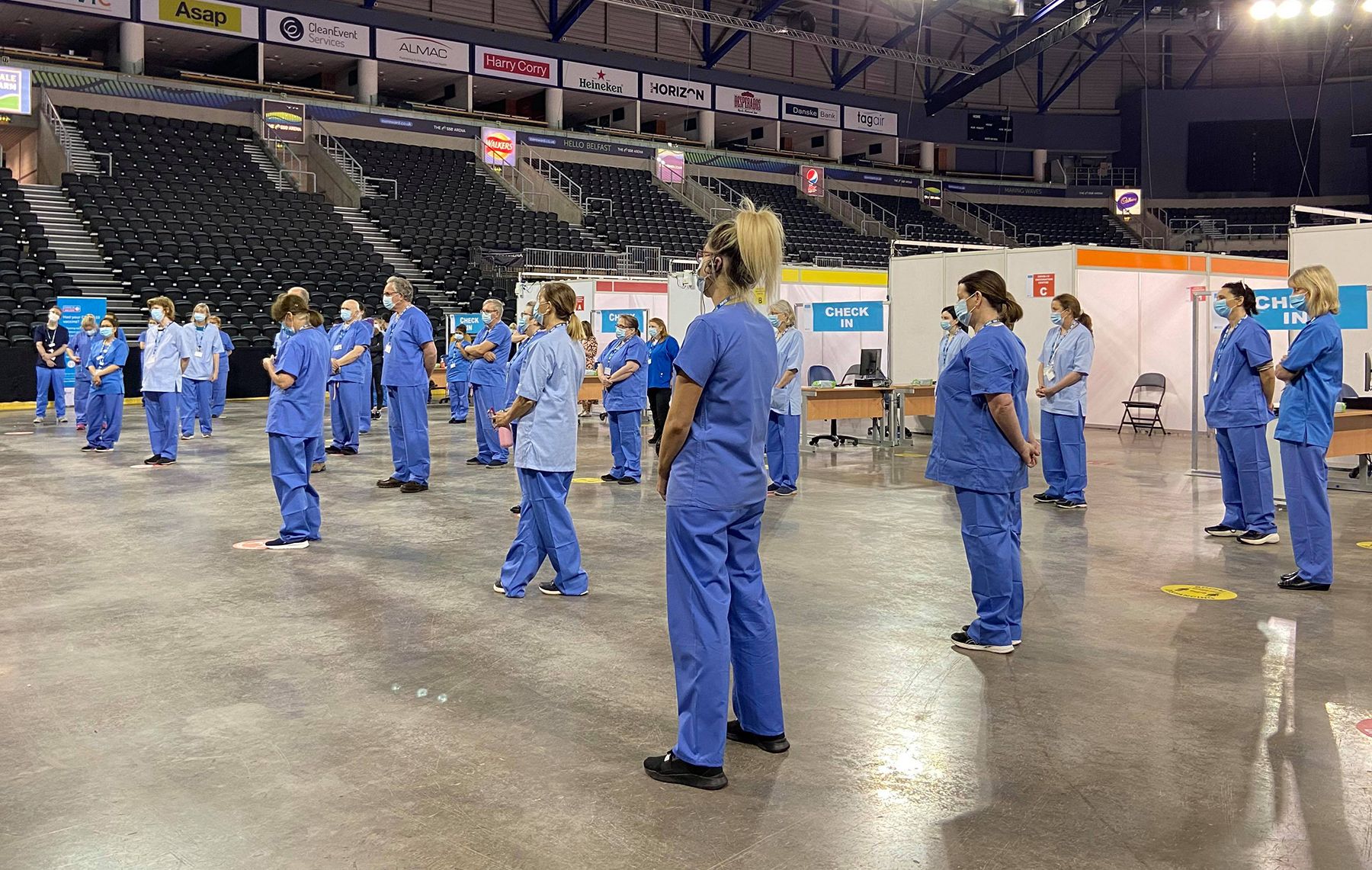
With the SSE Arena mass vaccine centre opening, Moderna vaccine expected from the United States towards the end of April, Glaxo to fill the Novartis vaccine and the expectation to send vaccine south, our thoughts may now turn to the long effects of Covid and how it might effect our health and social care services.
For some of us, Covid-19 can cause symptoms which may last for weeks or months after the infections seems to have gone.
This has been called Long Covid. Many people feel better in a few days or weeks and most in 12 weeks. About 5-36 per cent of patients get Long Covid but the chances of getting it do not seem to be linked to how ill one was when one was first infected.
Those who had mild symptoms can still get symptoms of Long Covid (2-15 per cent) which may include:
tiredness (98 per cent)
shortness of breath (93 per cent)
chest pain or tightness
headache (91 per cent)
memory problems
sleeping difficulties
palpitations
pins and needles
joint pains
depression and anxiety
tinnitus and earaches
nausea, diarrhoea, stomach aches, loss of appetite
high temperature
cough, headaches, sore throat, loss of smell or taste
skin rashes
Long Covid is thought not to be contagious and is caused by the body’s response to the virus continuing beyond the initial illness. To avoid passing the virus on to others, you should isolate for 10 days from your original symptoms or a positive test, or until the symptoms have gone.
You should pace yourself and break tasks down considering when best to do them, take frequent short rests, gradually increase exercise and lean forward on any walking stick or frame.
Be kind to yourself, connect with other people, have a daily routine and stay active.
Make notes to aid your memory, reduce distractions and make plans for complicated problems. Do flexibility exercises.
If you have had Covid and or develop any of the above symptoms you should discuss them with your general practice.
The health and social care services (HSCS) have had to respond to the needs of the pandemic and one wonders if the process will now be able to respond to overall health needs where various official reports have failed.
The omens are not good when nurses had to go on strike before the pandemic to get their pay rise. But, as we map our way out of the pandemic, only a 1 per cent rise is on the table here whereas in Scotland they have been offered 4 per cent. (An indication to those who still think Health and Social Care are a real part of the NHS, like NHS Scotland and NHS Cymru).
Professor Leonard Jason about #LongCovid and #pwme:
— Anil van der Zee © (@AnilvanderZee) March 27, 2021
“You have that whole group that is … basically trying to get their voice heard. They won’t be silenced."
We won't‼️‼️‼️‼️‼️‼️‼️‼️‼️‼️‼️‼️‼️‼️https://t.co/sJ7lV5kHyr
Vaccination has shown how important primary care services are and pilot multi-disciplinary teams are being rolled out in west Belfast.
After the pandemic elective care should be provided in dedicated centres and this might reduce waiting lists with hospitals focusing on emergency and complex care.
Such a transformation wrought by the pandemic would fulfil the Bengoa Report on transformation of care to better meet health needs.